End TB, Save lives
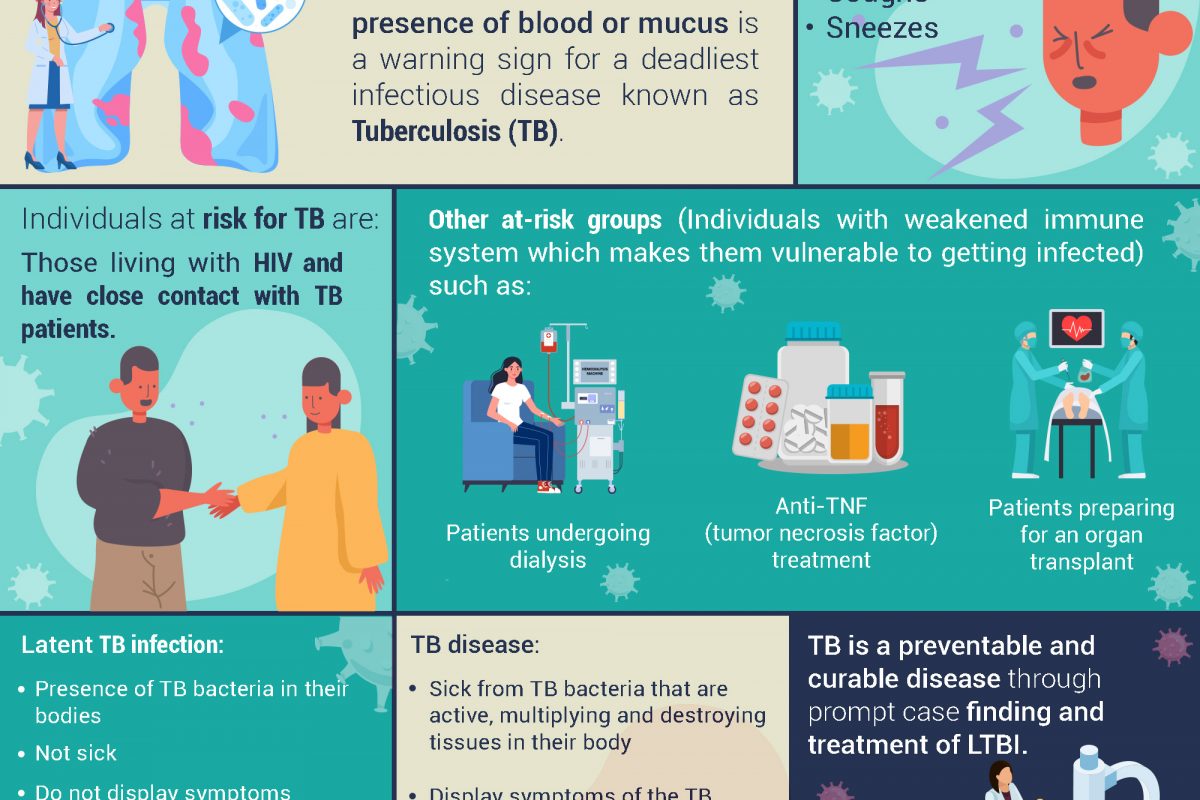
Persistent cough that lasts for more than 3 weeks with the presence of blood or mucus is a warning sign for a deadliest infectious disease known as Tuberculosis (TB).1, 2 TB bacteria spreads through air when someone with TB disease talks, coughs or sneezes.3 Individuals at risk for TB are those living with HIV and have close contact with TB patients and other at-risk groups such as patients undergoing dialysis, anti-TNF (tumor necrosis factor) treatment and patients preparing for an organ transplant.3 These individuals have weakened immune system which makes them vulnerable to getting infected.
Individuals with latent TB infection have TB bacteria in their bodies but are not sick, do not display symptoms or cannot spread the bacteria to others because the bacteria are not active. However, these individuals may develop TB disease in the future, hence, they are often prescribed treatment to prevent from developing TB disease. Whereas, individuals with TB disease are sick from TB bacteria that are active, multiplying and destroying tissues in their body. These individuals usually display symptoms of the TB disease and are able to spread the bacteria to others.6
TB is a preventable and curable disease, however, a person with TB can die if they do not get treatment on time.5, 6 Most TB cases are reported to progress from latent TB infection (LTBI) rather than local transmission, especially in those whose immune systems are weakened. Hence, the transmission of the infectious TB can be prevented through prompt case finding and treatment of LTBI as a crucial strategy to achieve the elimination of TB.7, 8, 9
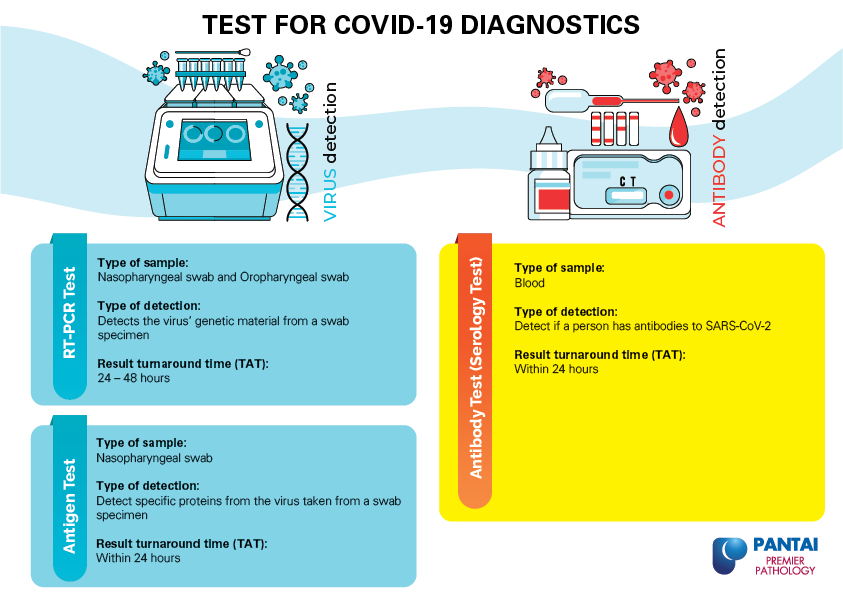
At Pantai Premier Pathology, we provide tests for Tuberculosis (TB):
- TB Serology Rapid Test
- MYCOBACTERIUM TB DNA PCR (FFPE TISSUE)
- MYCOBACTERIUM TB DNA PCR
- Mycobacterium TB Rifampin Resistance
- Mycobacterium Culture
- Mycobacterium Identification
- Mycobacterium Sensitivity
For more information on the tests provided, please contact us at +603-42809115 (Customer Service) or email us at info@premierpathology.com.my.
Reference
1- Signs & Symptoms. (n.d.). Centers for Disease Control and Prevention: Division of Tuberculosis Elimination. Retrieved March 8, 2021, from https://www.cdc.gov/tb/topic/basics/signsandsymptoms.htm
2- Tuberculosis (TB). (n.d.). NHS. Retrieved March 8, 2021, from https://www.nhs.uk/conditions/tuberculosis-tb/
3- How to Protect Ourselves from TB. (n.d.). World Health Organization. Retrieved March 11, 2021, from https://cdn.who.int/media/docs/default-source/campaigns-and-initiatives/world-tb-day-2020/how-to-protect-ourselves-from-tb.pdf?sfvrsn=ba76911a_2
4- Tuberculosis: General Information What is TB? (n.d.). Centers for Disease Control and Prevention: Division of Tuberculosis Elimination. Retrieved March 11, 2021, from https://www.cdc.gov/tb/publications/factsheets/general/tb.htm
5- Tuberculosis (TB). (n.d.-b). Centers for Disease Control and Prevention. Retrieved March 8, 2021, from https://www.cdc.gov/tb/publications/factsheets/general/tb.htm
6 – World Tuberculosis Day 2021: THE CLOCK IS TICKING. (n.d.). World Health Organization. Retrieved March 10, 2021, from https://www.who.int/campaigns/world-tb-day/world-tb-day-2021
7- Latent TB Infection and TB Disease. (2016). Centers for Disease Control and Prevention. https://www.cdc.gov/tb/topic/basics/tbinfectiondisease.htm
8- Lönnroth, K., Migliori, G. B., Abubakar, I., D’Ambrosio, L., De Vries, G., Diel, R., … & Ochoa, E. R. G. (2015). Towards tuberculosis elimination: an action framework for low-incidence countries. European Respiratory Journal, 45(4), 928-952.
9- Dobler, C. C., Martin, A., & Marks, G. B. (2015). Benefit of treatment of latent tuberculosis infection in individual patients. European Respiratory Journal, 46(5), 1397-1406.